Your child may still be eligible,
even if you don’t qualify for benefits!
Children who are under the age of 19 may still be eligible for Medi-cal coverage, even if their parents do not meet the requirements.
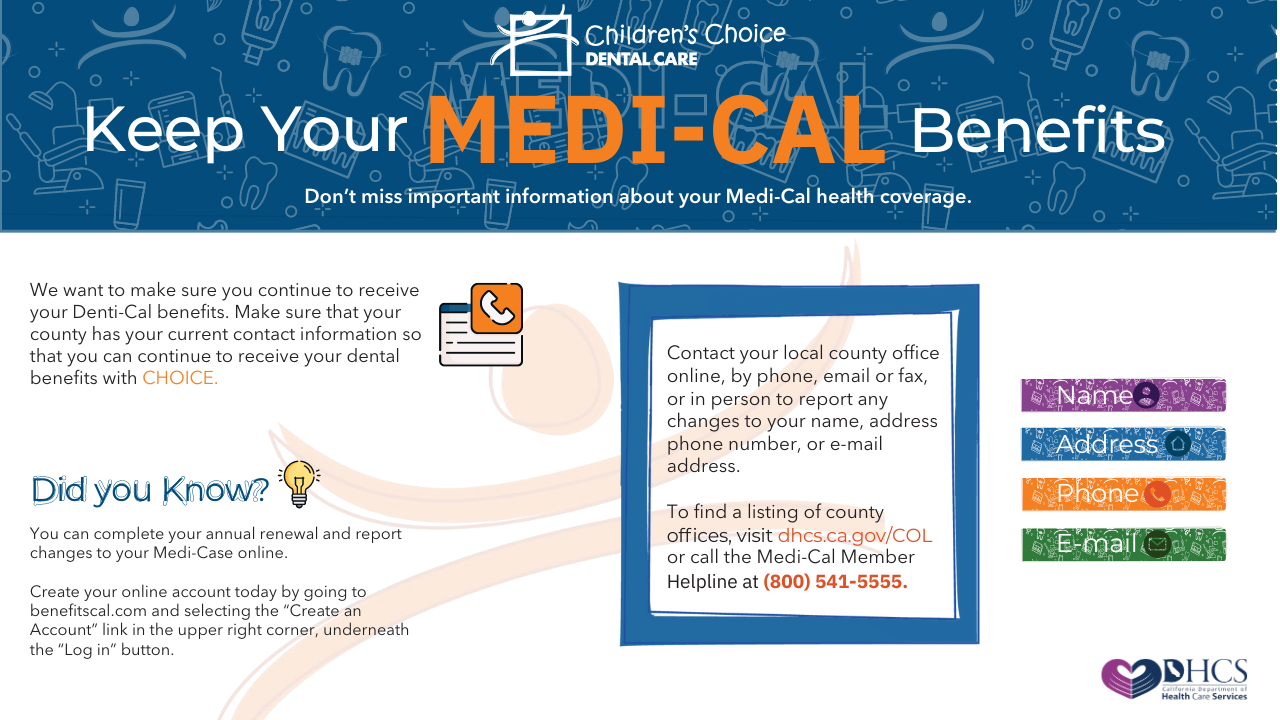
In January 2020, the U.S. Department of Health and Human Services (HHS) declared a Public Health Emergency (PHE) in response to the outbreak of COVID-19. Special rules were put in place during the COVID-19 PHE to allow more people to get access to and keep their Medi-Cal benefits. Prior to the PHE, California would review the information provided by beneficiaries and renew their participation in Medi-Cal if they still qualified. However, when the continuous coverage requirement expires at the end of the PHE, California will need to conduct a full redetermination for all beneficiaries who would have otherwise been subject to redetermination.
Even if you don’t qualify for benefits, your child is still eligible in most cases. In California, children under 19 years of age are eligible for full-scope Medi-Cal benefits regardless of their parent’s immigration status or eligibility, as long as they meet the necessary requirements.
DHCS is in Phase II of two phases to help beneficiaries be aware of the need to requalify for Medi-Cal. The current projected auto renewal rate is 25%. The state has projected a loss of coverage at about two-three million individuals. CMS is allowing a total of 14 months to resume normal eligibility redetermination.